Ketamine, a dissociative anaesthetic, has gained significant attention in recent years for its therapeutic potential. Ketamine infusion, at sub-anaesthetic doses, has been shown to be an effective treatment for various pain conditions, mental health (depression, PTSD, suicidal thinking), and addiction disorders.
Ketamine's unique pharmacological properties and rapid onset of action have made it an attractive option for patients who have not found relief from traditional therapies. Ketamine has shown promise in the management of acute and chronic pain, as well as the treatment of psychiatric disorders such as depression, PTSD, addiction, and suicidal ideation.
In this comprehensive guide, we will explore the many facets to ketamine infusion therapy. Our aim is to provide an understanding of ketamine's applications and limitations, enabling healthcare professionals and patients to make informed decisions about its use in specific clinical situations. By delving into the complexities of ketamine infusion therapy, we hope to contribute to the ongoing conversation surrounding this versatile and promising treatment option.
History of Ketamine
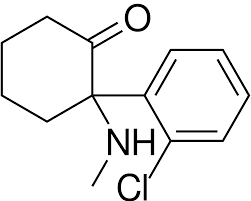
Ketamine was first synthesized in 1962 by Dr. Calvin L. Stevens, a chemist at Parke-Davis Laboratories, while searching for a safer alternative to phencyclidine (PCP) as an anesthetic agent. PCP, a potent NMDA receptor antagonist, had undesirable side effects such as severe hallucinations and agitation. Ketamine, also an NMDA receptor antagonist, was found to have a more favorable side effect profile compared to PCP, and it was patented in 1963.
Initial animal studies demonstrated ketamine's potential as an anesthetic, and human clinical trials began in the mid-1960s. The results of these trials showed that ketamine produced rapid-onset anesthesia with minimal respiratory depression, which was a significant advantage over other anesthetic agents available at the time. In 1970, the US Food and Drug Administration approved ketamine for use as a human anesthetic under the brand name Ketalar.
Ketamine as an Anesthetic
Ketamine gained popularity due to its unique anaesthetic and analgesic properties. It induces a state of "dissociative anesthesia," where the patient remains conscious but is disconnected from their sensory experiences. This was particularly useful in situations where intubation and mechanical ventilation were not feasible, such as in emergency settings, field surgery, and during the Vietnam War, where it was extensively used.
In addition to its use as a general anesthetic, ketamine has been utilized for procedural sedation, analgesia (pain relief), and as an adjunct to other anesthetic agents. Its ability to provide effective analgesia (pain relief) at sub-anesthetic doses has made it popular for use in painful procedures such as fracture reductions and dental surgery.
Emergence of Ketamine Infusion Therapy
In the late 1990s and early 2000s, researchers began to explore the potential of ketamine as a treatment for various pain conditions and psychiatric disorders. Early studies in pain medicine demonstrated that low-dose ketamine infusions could provide rapid and sustained relief for patients with chronic pain and neuropathic pain (measured by reduced pain score).
Around the same time, researchers discovered that ketamine could have rapid-acting antidepressant effects. A landmark study by Berman et al. (2000) found that a single sub-anesthetic dose of ketamine resulted in significant improvements in depressive symptoms within 4 hours, which persisted for several days. This finding was particularly significant given that traditional antidepressants typically take weeks to produce noticeable effects.
As more evidence accumulated regarding ketamine's analgesic effects in pain medicine and psychiatric disorders, the use of ketamine infusion therapy began to expand. Today, ketamine infusion therapy is increasingly used to treat a wide range of acute and refractory pain conditions (chronic pain syndromes, neuropathic pain, refractory chronic pain, chronic neuropathic pain, cancer pain, complex regional pain syndrome) as well as psychiatric disorders such as major depressive disorder, bipolar depression, treatment-resistant depression, post-traumatic stress disorder, and even addiction.
Mechanism of Action

NMDA Receptor Antagonism
The primary mechanism of action for ketamine is its antagonism of the N-methyl-D-aspartate (NMDA) receptor, a subtype of glutamate receptor. Glutamate is the primary excitatory neurotransmitter in the central nervous system (CNS) and plays a crucial role in synaptic plasticity, learning, and memory. By blocking NMDA receptors, ketamine reduces glutamatergic signaling, leading to decreased neuronal excitability and ultimately its anesthetic and pain relief effects.
Effects on Glutamate and GABA
While ketamine's antagonism of NMDA receptors is its primary mechanism of action, it also affects other neurotransmitter systems. Ketamine increases the release of glutamate in certain areas of the brain, leading to increased activation of another type of glutamate receptor called the α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor. This increased AMPA receptor activation is believed to be crucial for ketamine's rapid antidepressant effects.
In addition to its effects on glutamate signaling, ketamine also modulates the gamma-aminobutyric acid (GABA) system, the primary inhibitory neurotransmitter in the CNS. Ketamine has been shown to reduce the activity of GABAergic interneurons, leading to increased glutamate release and enhanced excitatory signaling in specific brain regions. This effect is thought to contribute to ketamine's ability to promote neuroplasticity and improve mood.
Influence on Neuroplasticity
Neuroplasticity refers to the ability of the brain to adapt and reorganize itself by forming new connections between neurons. Ketamine has been shown to promote neuroplasticity through multiple mechanisms, including increased activation of the mammalian target of rapamycin (mTOR) signaling pathway and increased expression of brain-derived neurotrophic factor (BDNF).
The mTOR signaling pathway is involved in regulating protein synthesis and cell growth, and its activation by ketamine is thought to promote synaptic strengthening and the formation of new neuronal connections. BDNF is a growth factor that supports neuronal survival, growth, and differentiation. In neuropathic pain models, increased BDNF levels following ketamine treatment may contribute to enhanced neuroplasticity and the rapid antidepressant effects observed in clinical studies.
Other Mechanisms
In addition to its effects on NMDA receptors, glutamate, GABA, and neuroplasticity, ketamine has been shown to interact with other neurotransmitter systems, such as the dopaminergic, serotonergic, and cholinergic systems. While these additional mechanisms are not yet fully understood, they may contribute to the diverse clinical effects of ketamine, including its effects on mood, cognition, and pain.
Furthermore, ketamine has anti-inflammatory properties, as it has been shown to suppress the production of pro-inflammatory cytokines and modulate immune cell activity. These anti-inflammatory effects may contribute to ketamine's efficacy in treating certain pain conditions (as measured by reduced pain score), such as complex regional pain syndrome (CRPS), as well as its potential therapeutic effects in psychiatric disorders with an inflammatory component, such as depression.
Pharmacology
Ketamine's pharmacological properties play a crucial role in its therapeutic effects and side effect profile.
Ketamine's absorption varies depending on the route of administration. Intravenous administration results in immediate and complete absorption, while oral and intranasal routes have lower and more variable absorption rates due to first-pass metabolism and mucosal barriers, respectively.
Once absorbed, ketamine rapidly distributes throughout the body, crossing the blood-brain barrier to exert its effects on the central nervous system (CNS). Ketamine is highly lipophilic, which facilitates its penetration into the brain and other tissues.
Ketamine is primarily metabolized in the liver by cytochrome P450 enzymes, with the primary metabolite being norketamine. Norketamine has some pharmacological activity, although it is less potent than ketamine itself. The rate of ketamine metabolism can be influenced by individual differences in liver enzyme activity, as well as interactions with other medications.
Ketamine and its metabolites are primarily excreted in the urine, with a small amount eliminated through the feces. The elimination half-life of ketamine varies depending on the route of administration and individual factors but is generally around 2-4 hours. This relatively short half-life contributes to the rapid offset of ketamine's effects following the cessation of infusion.
Administration
Ketamine can be administered through various routes, each with its own advantages and disadvantages depending on the clinical context and desired effects.

Intravenous
Intravenous (IV) administration is the most common route for ketamine infusion therapy. IV ketamine allows for rapid and precise dosing, with the drug directly entering the bloodstream for immediate systemic distribution. IV ketamine is particularly useful for anesthesia, pain management, and psychiatric indications, where fast onset and dose control are crucial.
Intranasal
Intranasal administration involves delivering ketamine as a nasal spray. This route offers a non-invasive option for patients and has shown promise for treating depression and other psychiatric disorders. Intranasal ketamine has a rapid onset, although the bioavailability is lower compared to IV administration, which may result in more variable and less predictable effects.
Oral
Oral ketamine involves swallowing a tablet or liquid formulation. This route is non-invasive and may be more convenient for some patients. However, oral ketamine has a slower onset, lower bioavailability, and more variable absorption compared to IV or intranasal administration, which may reduce its effectiveness in certain clinical contexts.
Sublingual
Sublingual administration involves placing a ketamine tablet or film under the tongue, where it dissolves and is absorbed through the oral mucosa. This route offers a non-invasive option with a rapid onset and higher bioavailability compared to oral administration. However, sublingual ketamine's effectiveness and safety have not been as extensively studied as other routes.
Intramuscular
Intramuscular (IM) administration involves injecting ketamine directly into a muscle, usually the thigh or upper arm. This route provides rapid onset and reliable absorption, making it a suitable option for anesthesia and emergency settings. However, IM injections can be more painful and invasive than other administration routes.
Ketamine dose
There are different dosages of ketamine used depending on the particular indication. You will often hear a comparisons that are made between anaesthetic doses (used in anaesthesia) and sub-anaesthetic doses (used in non-anesthetic indications) used to achieve certain ketamine concentrations. Ketamine is a medication that can be administered at different dosages depending on the intended use.
In anesthesia, a higher dose is used to induce and maintain anesthesia, while sub-anaesthetic doses are used for non-anesthetic indications such as depression, anxiety, PTSD, and chronic pain. Sub-anaesthetic low dose ketamine infusion have been shown to produce rapid and significant improvements in symptoms of depression, reduce symptoms of anxiety and PTSD, and improve quality of life for patients with chronic pain conditions. In anesthesia, a higher dose of ketamine is typically used to induce and maintain anesthesia, ranging from 1-2 mg/kg of body weight (sometimes higher). This is considered a supratherapeutic dose and is much higher than the sub-anaesthetic doses used for non-anesthetic indications.
Ketamine infusion therapy for mental health and chronic pain disorders is an area of ongoing research, and optimal dosing strategies, including dose cutoff thresholds, dose-response relationships, and infusion protocols, are yet to be definitively established. Ketamine for non-anaesthetic indications are typically administered at sub-anaesthetic doses, which are lower than the dose used in anesthesia. The available evidence suggests that low-dose ketamine infusions are typically effective, with dosages often ranging between 0.1 to 0.5 mg/kg per hour.
- Psychiatric treatment: Studies have shown that sub-anaesthetic doses of ketamine can produce rapid and significant improvements in depressive, anxiety and PTSD symptoms. These effects can last for several days to a week, and repeated treatments may be necessary to maintain the antidepressant effects.
- Pain treatment: Some studies have reported a dose-response relationship, indicating that higher doses of ketamine may provide greater pain relief (acute pain and chronic pain). However, higher doses also carry an increased risk of adverse effects. Therefore, finding the right balance between analgesic efficacy and minimizing side effects is crucial.
Regarding the infusion protocols, there is no clear consensus on the superiority of continuous infusions versus bolus administration or the optimal duration and frequency of ketamine infusions for acute pain and chronic pain management. Some studies have demonstrated the effectiveness of both single infusions and repeat or maintenance infusions in providing sustained pain reduction, but the ideal frequency and duration of treatment remain uncertain.
In summary, there is currently no definitive evidence for a therapeutic dose cutoff threshold, a dose-response relationship, or the superiority of specific infusion protocols for ketamine in the management of mental health and pain disorders. Further research is needed to establish optimal dosing strategies, taking into account the balance between efficacy and the risk of adverse effects. Individualizing treatment based on patient-specific factors, such as the type and severity of pain or psychiatric disorder, response to therapy, and tolerability, will continue to be essential in optimizing ketamine infusion therapy.
Clinical effects
Anaesthesia
Ketamine acts to induce a unique state of "dissociative anesthesia," characterized by profound analgesia (pain relief), sedation, and amnesia, while maintaining spontaneous respiration and airway reflexes. This is particularly advantageous in situations where intubation and mechanical ventilation are not feasible or desirable, such as in emergency medicine or field surgery. Ketamine can also be used as an adjunct to other anesthetic agents, improving analgesia (pain relief) and reducing the doses required of other pain medications, thereby minimizing their side effects.
Analgesia (Pain relief)
Ketamine has a potent analgesic effect, providing pain relief at sub-anesthetic doses. It's analgesic effect is effective in managing both acute and chronic pain, including neuropathic pain, which can be challenging to treat with traditional analgesics. Chronic pain conditions are a particular area where ketamine has shown utility in also reducing the associated pain medications. Ketamine's analgesic effects are thought to result from its NMDA receptor blockade, as well as its modulation of other neurotransmitter systems involved in pain processing, such as the dopaminergic and opioid systems.
Antidepressant, anti-suicidal and anti-PTSD effects
A growing body of research has demonstrated ketamine's rapid and robust antidepressant effects. A single sub-anesthetic dose of ketamine can lead to significant improvements in depressive symptoms within a few hours, and these effects can persist for days to weeks. This rapid onset of action is particularly significant given that conventional antidepressants typically take weeks to produce noticeable effects. Ketamine's antidepressant effects are believed to be mediated through its actions on glutamate and GABA, as well as its promotion of neuroplasticity.
Ketamine has shown promise in treating bipolar depression, a form of depression that occurs in the context of bipolar disorder. Clinical trials have reported rapid and significant reductions in symptoms of depression following ketamine administration in patients with bipolar depression. However, larger and more long-term studies are needed to confirm its safety and efficacy in this population.
Ketamine has shown promise as an intervention for suicidal ideation. Multiple studies have reported rapid reductions in suicidal thoughts following ketamine administration, with some patients experiencing relief within a few hours. This effect is especially important considering the urgent need for fast-acting interventions in individuals at risk for suicide.
Ketamine has demonstrated efficacy in reducing symptoms of post-traumatic stress disorder (PTSD) in several clinical trials. Its rapid effects on mood, anxiety, and intrusive thoughts may be particularly beneficial for individuals with PTSD. The exact mechanisms underlying ketamine's effects on PTSD are not yet fully understood but may involve its actions on glutamate, GABA, and neuroplasticity, as well as its potential to disrupt the reconsolidation of traumatic memories.
Effects on Addiction
Preliminary research has suggested that ketamine may have potential as a treatment for addiction, particularly for alcohol and drug use disorders. Studies have reported reductions in craving and relapse rates following ketamine administration in individuals with substance use disorders. The mechanisms underlying ketamine's potential effects on addiction are not yet fully understood but may involve its actions on the glutamatergic and dopaminergic systems, as well as its promotion of neuroplasticity, which could facilitate the formation of new, healthier habits
Clinical indications
Ketamine has a variety of clinical indications due to its unique pharmacological properties. Not least of which are its analgesic effect and psychoactive properties. Some of the most common indications for ketamine treatment include:
- Anesthesia and analgesia (i.e. pain relief)
- Acute pain
- Spontaneous pain
- Neuropathic pain conditions (pain due to damage or lesion to the somatosensory nervous system e.g. spinal cord injury and nerve injury)
- Other chronic non-cancer pain conditions and pathological pain states: fibromyalgia pain, complex regional pain syndrome (or chronic regional pain syndrome, CRPS), post-herpetic neuralgia, irritable bowel syndrome (IBS), spinal cord injury related pain, phantom limb pain, prevent chronic pain
- Nociplastic pain
- Central sensitisation
- Cancer pain (cancer patients with refractory cancer pain)
- Opioid induced hyperalgesia & opioid use reduction
- Treatment-resistant major depression (TRD)
- Bipolar depression
- Suicidal ideation
- Post-traumatic stress disorder (PTSD)
- Anxiety disorders: generalized anxiety disorder (GAD) and social anxiety disorder (SAD).
- Obsessive-compulsive disorder (OCD)
- Addiction disorders: alcohol and opioid use disorders
- Migraine and other headache disorders
It's important to note that the use of ketamine for some of these indications is still considered off-label, and more research is needed to fully understand its safety and efficacy in these settings. More research is also needed to establish optimal dosages and treatment protocols. Ketamine nonetheless offers a promising alternative for individuals who have not responded well to traditional treatments or who are seeking rapid relief of symptoms. Consultation with a healthcare professional is essential to determine if ketamine is an appropriate treatment option for a specific patient.
For a more in-depth review on these indications and their effectiveness see our article How effective are ketamine infusions in pain and psychiatric management?. Also go to our piece on ketamine and depression at https://anodynegroup.com.au/blogs/ketamine-and-depression/.
Side effects & safety considerations
While ketamine has demonstrated effectiveness in various clinical applications, it is essential to be aware of its potential side effects. Below we provide a brief summary, but please go to our article Ketamine Side Effects and Safety Considerations: A Comprehensive Exploration for a more in depth review of ketamine and its side effects.
Common Side Effects
Common side effects of ketamine include dizziness, drowsiness, nausea, vomiting, visual disturbances (e.g. double and/or blurry vision), constipation, headaches, trouble passing urine, and transient increases in blood pressure and heart rate. Infection at the site of intravenous ketamine infusions, while not common, is an important consideration. These side effects are generally mild and short-lived, resolving spontaneously as the drug's effects wear off. In some cases, adjunct medications may be used to minimize these side effects during treatment.
Neuropsychiatric Side Effects
Ketamine can cause psychiatric side effects, such as euphoria or dysphoria, jerky movements, hallucinations, vivid dreams, and feelings of dissociation or "out-of-body" experiences. These effects are more common at higher doses and are typically transient, resolving as the drug is metabolized. To minimize the risk of psychiatric side effects, lower doses of ketamine and a calm, supportive treatment environment are often employed.
Cardiovascular Side Effects
Ketamine can cause transient increases in blood pressure, heart rate, and cardiac output, particularly during the initial stages of administration. These effects are usually well-tolerated and short-lived but may be of concern in patients with pre-existing cardiovascular disease. In these cases, careful monitoring and dose adjustment may be necessary to minimize the risk of adverse cardiovascular events.
Interactions with Other Medications
Ketamine can interact with other medications, potentially increasing the risk of side effects or reducing the efficacy of either drug. Of particular concern are interactions with CNS depressants, such as benzodiazepines, opioids, and alcohol, which can increase the risk of respiratory depression and sedation. It is essential to inform your healthcare provider of all medications you are taking before undergoing ketamine therapy.
Long term side effects
Long-term use of ketamine, particularly at high doses or when used recreationally, may be associated with a range of potential side effects. It is important to note that the long-term side effects of ketamine in a controlled clinical setting are less well-established, as most studies have focused on its short-term safety and efficacy. However, some potential long-term side effects of ketamine use may include:
Cognitive impairments: Chronic ketamine use may lead to deficits in memory, attention, and executive functioning. These cognitive impairments may be reversible upon cessation of ketamine use, but more research is needed to determine the extent of potential cognitive recovery.
Urinary symptoms and bladder toxicity: Long-term ketamine use has been linked to lower urinary tract symptoms, including increased urgency and frequency of urination, pain during urination, and blood in the urine. In severe cases, ketamine-associated cystitis may occur, which can lead to irreversible bladder damage.
Liver toxicity: Although rare, chronic ketamine use has been associated with liver toxicity and elevated liver enzymes. The risk of liver damage increases with higher doses and more frequent use of ketamine.
Psychological effects: Long-term ketamine use may exacerbate pre-existing mental health disorders or increase the risk of developing new psychiatric symptoms, such as anxiety, depression, or psychosis.
Tolerance and dependence: Prolonged use of ketamine can lead to the development of tolerance, requiring higher doses to achieve the desired effects. Additionally, psychological dependence may develop, with users experiencing cravings and compulsive drug-seeking behavior.
Withdrawal symptoms: Some individuals who use ketamine chronically may experience withdrawal symptoms upon discontinuation, including anxiety, irritability, insomnia, and restlessness.
It is essential to recognize that the long-term side effects of ketamine are more commonly associated with recreational use or abuse (i.e. ketamine abusers) and may not be as prevalent in controlled clinical settings. When used under the guidance of a healthcare professional and following appropriate treatment protocols, the risk of long-term side effects may be significantly reduced. However, more research is needed to better understand the long-term safety of ketamine when used for clinical purposes.
Ketamine safety
Ketamine has a long history of use in various clinical settings, with a generally favorable safety profile. However, its safety may be influenced by the specific context in which it is used and the patient population being treated.
Anaesthesia: Ketamine has a well-established safety profile as an anesthetic agent, with a low incidence of severe adverse events. Its unique properties, such as maintaining spontaneous respiration and airway reflexes, make it particularly advantageous in situations where intubation and mechanical ventilation are not feasible or desirable.
Pain management: Ketamine's safety in pain management is generally favorable, with most side effects being mild and transient. When used at sub-anesthetic doses, the risk of severe side effects is reduced, and careful patient selection and monitoring can further enhance safety.
Psychiatric management: Ketamine's safety profile in mental health treatment, particularly for treatment resistant major depression and PTSD, has been promising, with most side effects being mild and transient. However, there is a need for further research on the long-term safety and efficacy of ketamine therapy in mental health disorders.
Addiction treatment: Preliminary research suggests that ketamine infusions may have potential as a treatment for addiction, but further research is needed to establish its safety and efficacy in this context. Special consideration should be given to the risk of drug abuse and dependence, given ketamine's psychoactive properties.
Special Populations
Certain populations, such as pregnant or breastfeeding individuals, children, and those with pre-existing cardiovascular or psychiatric conditions, may be at increased risk for adverse effects from ketamine and may not be an appropriate ketamine group of patients. In these cases, careful patient selection, dose adjustment, and monitoring may be necessary to minimize risks and ensure safe and effective treatment for this ketamine group.
Contraindications
While ketamine has demonstrated effectiveness and safety in various clinical applications, certain conditions or circumstances may preclude its use. Contraindications can be classified as absolute, where ketamine use is strictly prohibited, or relative, where the risks and benefits should be carefully weighed before treatment.
Absolute contraindications:
- Known hypersensitivity or allergy to ketamine or its components: Patients with a history of severe allergic reactions to ketamine should not receive the drug.
- Severe, uncontrolled hypertension or history of hypertensive crisis: Ketamine produced transient hypertension, which may be dangerous for patients with poorly controlled hypertension.
- High-risk coronary vascular disease, aortic dissection or cerebral aneurysm: The increase in blood pressure associated with ketamine administration could potentially lead to the rupture of a pre-existing aortic dissection or cerebral aneurysm.
- Refusal or inability to provide informed consent to treatment
Relative contraindications:
- Cardiovascular disease: Patients with pre-existing cardiovascular conditions, such as coronary artery disease, unstable angina, or heart failure, may be at increased risk for complications related to ketamine-induced increases in blood pressure and heart rate. Careful monitoring and dose adjustment may be necessary in these cases.
- Psychiatric disorders: Individuals with a history of psychosis, psychotic related conditions, mania, or dissociative disorders may be at increased risk for exacerbation of symptoms due to ketamine's psychoactive effects. The risks and benefits of ketamine treatment should be carefully weighed for these patients.
- Neurocognitive disorders: Individuals delirium, dementia or cognitive impairment may be at increased risk for exacerbation of symptoms due to ketamine's psychoactive effects. Together with the long term side effects of ketamine related to worsening cognition. The risks and benefits of ketamine treatment should be carefully weighed for these patients.
- Addiction: active substance abuse and/or intoxication with alcohol or other substances (in particular ketamine abusers)
- Endocrine disorders: including phaeochromocytoma and hyperthyroidism
- Glaucoma or increased intraocular pressure: Ketamine can cause an increase in intraocular pressure, which may be problematic for patients with glaucoma or other eye conditions associated with elevated intraocular pressure.
- Elevated intracranial pressure: including secondary traumatic brain injuries or tumours
- Pregnancy and breastfeeding: The safety of ketamine use during pregnancy and breastfeeding is not well established, and its use should be carefully considered in consultation with a healthcare professional.
- Concurrent use of CNS depressants: Ketamine can interact with other medications that depress the CNS, such as benzodiazepines, opioids, and alcohol, increasing the risk of respiratory depression and sedation. Caution should be exercised when using ketamine in combination with these substances.
- Liver disease: Ketamine is primarily metabolized in the liver, and patients with significant liver disease may have altered metabolism and clearance of the drug, potentially increasing the risk of adverse effects. Ketamine can also increase liver blood flow which could further exacerbate liver disease related problems in these patients. Close monitoring and dose adjustments may be necessary in these cases.
Treatment process
The ketamine treatment process involves several steps to ensure that patients receive safe, effective, and individualized care.
Assessment
Before initiating ketamine infusions, a comprehensive evaluation of the patient's medical history, current medications, and any contraindications is essential. While there is no standardized pre-infusion testing protocol, several tests and assessments may be considered to ensure the safety and appropriateness of ketamine therapy:
Physical examination: A thorough physical examination should be performed to evaluate the patient's general health status and identify any potential concerns that may affect the safety or efficacy of ketamine infusion therapy.
Baseline vital signs: Monitoring baseline vital signs, including blood pressure, heart rate, respiratory rate, and oxygen saturation, can help identify any underlying issues that need to be addressed before ketamine administration.
Electrocardiogram (ECG): An ECG may be considered for patients with a history of cardiac disease, arrhythmias, or risk factors for cardiovascular events, as ketamine can increase heart rate and blood pressure.
Blood and urine tests: Basic blood tests, including a complete blood count (CBC), electrolyte panel, and liver and kidney function tests, and a urinalysis, may be performed to assess the patient's overall health and ensure they can safely receive ketamine treatment. Additional blood tests, such as coagulation studies, may be considered for patients with a history of bleeding disorders or those taking anticoagulant medications.
Pregnancy test: A pregnancy test should be performed for women of childbearing age, as ketamine's safety during pregnancy has not been established.
Psychiatric evaluation: A psychiatric evaluation may be considered for patients with a history of psychiatric disorders, as ketamine can potentially exacerbate certain mental health conditions or trigger hallucinations and dissociative experiences.
Medication review: A thorough review of the patient's current medications is essential to identify potential drug interactions and adjust dosages as necessary.
Ultimately, the specific tests and assessments required will depend on the patient's individual circumstances, risk factors, and the judgment of the treating clinician. It is important to ensure that all necessary precautions are taken to optimize the safety and efficacy of ketamine infusion therapy.
Treatment Planning
Based on the initial assessment, a treatment plan is developed that outlines the specific goals, dosing, frequency, and duration of ketamine infusions. This plan is tailored to the patient's unique needs and may be adjusted over time as needed. The treatment team will closely monitor the patient's progress and response to the treatment.
Monitoring
During ketamine infusions, patients are closely monitored by medical professionals to ensure their safety and comfort. Vital signs, including blood pressure, heart rate, and oxygen saturation, are routinely checked, and any adverse effects are promptly addressed. The treatment team may adjust the dosing or infusion rate to optimize the treatment's efficacy and minimize side effects.
Post-treatment care
Following ketamine infusions, patients may require post-treatment care to ensure their ongoing safety and well-being. This may involve a brief period of observation, particularly after the initial treatment, to monitor for any lingering side effects or complications. The treatment team will also work with the patient to develop a follow-up plan, which may include additional ketamine treatments or other therapies, depending on the patient's needs and response to treatment.
Long-term care
Long-term monitoring of ketamine infusions is essential to ensure its safety, efficacy, and tolerability in managing chronic pain or other conditions. While there is no standardized long-term monitoring protocol, the following considerations may be helpful in guiding patient care:
Pain management & assessment: Regularly evaluate the patient's pain levels and overall quality of life to assess the effectiveness of ketamine therapy and make any necessary adjustments to the treatment plan.
Side effects and tolerability: Monitor the patient for any adverse effects, both short-term (e.g., dizziness, nausea, hallucinations) and long-term (e.g., cognitive impairment, urinary symptoms, dependence). Early detection and management of side effects can help optimize the safety and tolerability of ketamine infusion therapy.
Mental health assessment: Regularly assess the patient's mental health, as ketamine has been associated with psychiatric symptoms, including mood changes, hallucinations, and dissociative experiences. Monitor patients with a history of psychiatric disorders more closely, as ketamine therapy may exacerbate their condition.
Substance use and abuse risk: Evaluate the patient's risk of substance abuse and monitor for any signs of misuse or dependence, as ketamine has the potential for abuse.
Cardiovascular monitoring: Periodically assess the patient's blood pressure, heart rate, and other cardiovascular parameters. This monitoring may be particularly important for patients with pre-existing cardiovascular conditions or risk factors.
Liver and kidney function: Regularly monitor liver and kidney function, as ketamine is metabolized by the liver and excreted by the kidneys. Long-term use of ketamine may potentially cause liver or kidney toxicity in some patients.
Bladder function: Regularly monitor bladder function, usually through urinalysis, as long-term use of ketamine may potentially bladder toxicity in some patients.
Interactions with other medications: Continuously review the patient's medications to identify potential drug interactions and adjust dosages as necessary.
Follow-up appointments: Schedule regular follow-up appointments with the patient to discuss their progress, address any concerns or questions, and provide support throughout the course of ketamine infusion therapy.
The specific long-term monitoring requirements will depend on the patient's individual circumstances, the underlying condition being treated, and the treating clinician's judgment. Close collaboration between the patient and healthcare provider is crucial for ensuring the safe and effective use of ketamine infusion therapy over the long term.
Treatment considerations
Ketamine treatment offers significant potential for a variety of medical conditions, particularly in cases where conventional therapies have proven ineffective. However, as with any medical intervention, it is essential to carefully consider various factors to ensure the safety and efficacy of ketamine therapy.
Use of other medications during ketamine infusions
In order to manage potential adverse events related to ketamine infusions, it is crucial to have pre-emptive medications readily available as rescue treatments. The following medications can be considered for this purpose:
Benzodiazepines: Agents like midazolam or lorazepam can be used to manage anxiety, agitation, or restlessness during ketamine infusions. They may also help counteract the hallucinations or dissociative experiences that some patients may experience.
Antiemetics: Nausea and vomiting are common side effects of ketamine infusions. Having antiemetic medications, such as ondansetron or metoclopramide, on hand can help manage these symptoms.
Antihypertensives: Ketamine can cause transient hypertension. Medications like clonidine can be administered to manage the hypertensive episode.
Oxygen: Oxygen should be readily available in cases of respiratory depression or hypoxia during the ketamine infusion.
Cardiac medications: In case of arrhythmias or other cardiac events, having appropriate cardiac medications and equipment available is crucial.
The specific medications required will depend on the patient's individual risk factors, medical history, and the treating clinician's judgment. It is essential to closely monitor the patient throughout the ketamine infusion and be prepared to manage any potential adverse events that may arise.
Staff training and experience
Ketamine is a potent medication with potential side effects and risks. Therefore, healthcare professionals must have specialized training in their clinical practice and expertise to administer ketamine safely and effectively. There is a significant difference between health professionals (e.g. pain physician, psychiatrist, anaesthetist) with not all having the expertise to manage ketamine or intravenous infusions. Here are some of the training requirements for healthcare staff to provide ketamine and intravenous infusions safely:
Education and Training: Healthcare professionals (including a pain physician) who administer ketamine should have specialized training and education on the safe use of the medication, including the proper dosing, administration techniques, and monitoring for side effects. There are significant differences in the administration techniques warranting specialised training (e.g. intravenous infusions/IV ketamine vs oral or subcutaneous).
Certification and Licensure: Healthcare professionals (including a pain physician)are required to have specific certification to administer ketamine. Healthcare professionals should ensure that they meet the requirements and have the appropriate certifications and licenses to administer ketamine (including IV ketamine and intravenous infusions) safely.
Clinical Experience: Healthcare professionals (including a pain physician) who administer ketamine should have clinical experience in anesthesia, pain management, and psychiatry to ensure that they have the knowledge and expertise to manage potential side effects and risks associated with ketamine therapy (including intravenous infusions and IV ketamine).
Ongoing Education: Healthcare professionals who administer ketamine should participate in ongoing education and training to stay up-to-date on the latest research, best practices, and safety considerations.
Collaborative Care: Healthcare professionals who administer ketamine should work collaboratively with other healthcare providers, including anesthesiologists, pain management specialists, psychiatrists, and primary care providers, to ensure that patients receive comprehensive care and monitoring.
In conclusion, healthcare professionals who administer IV ketamine infusions should have specialized education, certification, and clinical experience to ensure that they can provide safe and effective care to patients. Ongoing education and collaboration with other healthcare providers are also essential to ensure that patients receive comprehensive care and monitoring.
Treatment setting

Ketamine infusions (Including IV ketamine) can be provided in various settings, depending on the patient's needs and the specific application of the therapy.
Inpatient: inpatient ketamine infusions are typically provided in a hospital or specialized treatment center. This setting may be appropriate for patients requiring intensive monitoring, those with unstable medical or psychiatric conditions, or those undergoing ketamine treatment as part of a broader inpatient treatment program.
Outpatient: can be provided in a clinic or outpatient treatment center. This setting is suitable for patients who are medically stable and can safely receive ketamine treatment without the need for ongoing inpatient care.
Ambulatory: refers to treatment provided in a specialized outpatient setting designed to accommodate patients during the infusion process. Patients in this setting receive treatment and monitoring but return home or to another care setting following the ketamine infusions.
Home infusion: an emerging treatment setting for ketamine therapy, in which patients receive ketamine treatment in the comfort of their own homes under the supervision of medical professionals. This option may be suitable for patients who are medically stable and have a supportive home environment. However, it is crucial to ensure that proper safety measures and monitoring are in place during home infusion.
Limitations
While ketamine has shown promise in various clinical applications, particularly in treating treatment-resistant mental health disorders and pain management, it does have some limitations and important treatment considerations to consider.
Short-term effects: Although ketamine can provide rapid relief from symptoms such as depression or anxiety, the effects may be short-lived, requiring repeated treatments to maintain the benefits.
Treatment Frequency and Duration: The frequency and duration of ketamine infusions will depend on the individual patient's needs and response to treatment. Typically, patients receive a series of infusions over a few weeks, with the frequency gradually decreasing over time. The treatment plan should be tailored to the patient's specific needs and condition.
Monitoring and Support: Patients receiving ketamine infusions should be closely monitored during and after treatment to manage any potential side effects or adverse reactions. Depending on the patient's individual needs and medical history, additional support such as psychotherapy or medication management may also be recommended. The healthcare provider should also monitor the patient's response to treatment and adjust the treatment plan as necessary.
Safety concerns: Pre-existing cardiovascular conditions are a risk given the cardiovascular effects of ketamine. Some patients may experience negative psychological effects such as anxiety, panic, dissociative features, or distress. Ketamine use may also exacerbate symptoms in individuals with a history of psychosis, mania, dissociative or other psychiatric disorders.
Long term safety: While the short-term safety profile of ketamine is relatively well-established, more research is needed to determine its long-term safety, particularly when used repeatedly or in conjunction with other treatments.
Potential for abuse: Although ketamine is considered to have a lower potential for abuse compared to other substances, it can still lead to psychological dependence and compulsive use in some individuals. In particular are chronic ketamine abusers and people with a history of substance use disorders.
Limited availability: Access to ketamine therapy can be limited due to a lack of trained providers, insurance coverage, or regulatory constraints in certain countries.
Treatment Setting: Ketamine infusions should be administered in a specialized treatment center with trained staff who can monitor patients during and after the infusion. The treatment center should also have the necessary equipment and medication to manage any potential adverse effects. The patient's comfort and safety should be the primary concern during treatment.
Lack of standardised protocols: There is still considerable variability in ketamine treatment protocols, such as dosing regimens, administration routes, and the integration of psychotherapy. More research is needed to establish standardized, evidence-based practices.
Drug interactions: Ketamine may interact with other medications, leading to potential adverse effects or reduced treatment efficacy. Patients must inform their healthcare provider of all medications they are taking to minimize risks.
Suitability & eligibility: Ketamine is not suitable for all patients, and it is contraindicated in certain cases, such as those with a history of severe allergies to ketamine or related compounds. Ketamine infusions are generally reserved for patients who have not responded to conventional treatments or who have treatment-resistant conditions. Eligibility criteria may vary depending on the specific condition being treated.
Cost: Ketamine infusions can be expensive, and insurance coverage may vary. Outpatient ketamine infusions are typically self-funded as there are no Medicare mechanisms in place to fund treatment outside of anaesthesia. DVA, workers compensation and motor vehicle accident insurers will variably support treatment costs. Inpatients treatment can sometimes be covered under private health insurance, but this is not always the case.
Overall, ketamine infusions can be an effective treatment option for pain, mental health, and addiction disorders in eligible patients. However, it requires careful consideration of the patient's individual needs and medical history, a specialized treatment setting, and close monitoring during and after treatment. Ongoing research is also needed to refine its use and enhance its potential benefits for patients in need.
Special considerations
Specialized treatment approaches for ketamine therapy aim to optimize outcomes by tailoring interventions to individual patient needs and specific medical conditions. These approaches involve interdisciplinary collaboration among healthcare professionals with expertise in ketamine administration, ensuring the highest standards of care and safety.
By utilizing evidence-based practices and personalized treatment strategies, specialized treatment approaches can enhance the therapeutic potential of ketamine while minimizing adverse effects and risks.
Legal status of ketamine in Australia
In Australia, ketamine is a Schedule 8 drug, meaning that it is classified as a controlled substance and can only be used for specific medical purposes. Ketamine is primarily used in Australia as an anesthetic in hospitals and clinics.
Ketamine when used for the treatment of psychiatric and pain conditions, including treatment resistant major depression, PTSD, and chronic pain, is considered an off label treatment. However, the off-label use of ketamine for these conditions is not currently approved by the Therapeutic Goods Administration (TGA) in Australia, and there are no specific guidelines for its use in these contexts.
In recent years, the use of ketamine for the treatment of certain psychiatric and pain conditions has generated significant interest, and some healthcare providers in Australia are using ketamine off-label to treat these conditions. However, the use of ketamine in this way is controversial, and there are concerns about its safety and potential long-term effects.
Overall, while ketamine is legal for medical use in Australia, its use for specific psychiatric and pain conditions is currently off-label and not approved by the TGA. Patients who are considering ketamine for off-label use should consult with a healthcare provider who has expertise in the use of ketamine and is familiar with the legal and regulatory requirements for its use in Australia.
Ketamine as an “off-label” treatment
It is important to note that in Australia ketamine is only approved for anaesthesia. This means that for all other indications ketamine is used as an off-label treatment. This means that it is being used to treat a condition for which it is not officially approved by regulatory agencies. In the case of ketamine, it has been used off-label to treat treatment resistant major depression, post-traumatic stress disorder (PTSD), bipolar disorder, and chronic pain conditions, among others.
The use of ketamine for treatment resistant major depression, in particular, has gained widespread attention as studies have demonstrated its rapid and robust antidepressant effects. However, the FDA and TGA have only approved ketamine for use as an anesthetic, and its use for treating depression remains off-label.
Off-label use of medications is not uncommon in medicine, and it is legal for healthcare providers to prescribe medications off-label when they believe it to be in the best interest of the patient. However, off-label use can also carry potential risks and uncertainties, as the safety and effectiveness of the medication for that particular condition may not be fully understood.
Patients considering ketamine as an off-label treatment should discuss the potential risks and benefits with their healthcare provider, including the possible side effects and the potential for drug interactions. They should also be informed about the lack of official approval for their specific condition and the uncertainties that come with off-label use.
In summary, ketamine has been used off-label to treat several conditions, including depression, anxiety, PTSD, bipolar disorder, and chronic pain. While off-label use of medications is legal and not uncommon, patients should discuss the potential risks and uncertainties with their healthcare provider before considering ketamine as an off-label treatment.
Please see our article Off-Label Prescribing in Medicine: A Deep Dive into the Australian Health System for more information on off-label prescribing in medicine.
Ketamine as a psychedelic
Ketamine, a dissociative anesthetic, has gained attention as a psychedelic due to its unique psychoactive properties. Its ability to induce dissociative states, hallucinations, and ego dissolution has sparked interest in its potential use for personal growth, self-exploration, and spiritual experiences.
While ketamine's effects differ from those of classic psychedelics like LSD and psilocybin, it has shown promise as an adjunct to psychotherapy, particularly for treatment-resistant mental health disorders. Despite the potential benefits, ketamine's use as a psychedelic also presents risks and safety concerns, necessitating further research and responsible use in therapeutic settings.
Please see our article Ketamine: Exploring Its Potential as a Psychedelic for more information on ketamine as a psychedelic.
Ketamine assisted therapy
Ketamine-assisted therapy is an innovative mental health treatment that combines the psychoactive properties of ketamine with the guidance of trained therapists. This approach has demonstrated promise in treating treatment-resistant disorders such as depression, anxiety, and PTSD by facilitating deeper emotional healing and personal growth.
Patients undergoing ketamine-assisted therapy receive controlled doses of the drug, enabling them to explore emotions, thoughts, and memories that may be difficult to access in conventional therapy sessions. While this modality offers potential benefits, it is essential to remain aware of the risks and safety considerations and continue researching its applications and efficacy.
Please see our article Ketamine-Assisted Therapy: Unlocking New Avenues for Mental Health Treatment for further discussion on ketamine as a psychedelic.
Ketamine vs Esketamine (Spravato) in depression
Intravenous ketamine infusion and Spravato (esketamine) nasal spray are both innovative treatments for depression, particularly for patients with treatment-resistant depression. While both treatments share a similar mechanism of action and have demonstrated efficacy in alleviating depressive symptoms, they differ in their administration methods, side effects, accessibility, and cost.
Intravenous ketamine infusion is administered intravenously in a specialized treatment center and may provide more robust and rapid antidepressant effects. Spravato is self-administered as a nasal spray under the supervision of a healthcare professional in a certified treatment center and may be more convenient and accessible for some patients.
Ultimately, the choice between the two treatments should be made in consultation with a healthcare professional, taking into account individual needs, medical history, and potential risks.
Please see our article Ketamine Infusion vs. Spravato: A Comparison of Two Innovative Treatments for Depression for further discussion on ketamine vs esketamine.
Working with your health professional
When considering the use of ketamine as a treatment, it is essential to work closely with your healthcare provider. Ketamine is a powerful medication with potential side effects and risks, and there are still a lot of unknowns around its use. Therefore, it should only be used under the guidance of trained medical professionals (e.g. pain physician). Some of these reasons are listed below.
Safety: Ketamine can cause several side effects, including dizziness, confusion, hallucinations, and hypertension. A healthcare provider can monitor your response to the medication and adjust the dosage as needed to minimize the risk of adverse effects.
Optimal Dosage: The optimal dosage of ketamine for different conditions is still being studied, and it may vary depending on the individual patient. A healthcare provider can work with you to determine the appropriate dosage and treatment frequency based on your medical history and response to the medication.
Monitoring: Ketamine can produce rapid and significant improvements in symptoms, but it is essential to monitor your progress to determine the efficacy and potential side effects. A healthcare provider can monitor your response to the medication and adjust the treatment plan as needed.
Drug Interactions: Ketamine can interact with other medications, including antidepressants and opioids. A healthcare provider can review your medication list and make any necessary adjustments to avoid potentially dangerous interactions.
Follow-Up Care: Ketamine is often administered through an infusion, and follow-up care is essential to monitor the long-term effects of the treatment. A healthcare provider can work with you to develop a follow-up care plan that includes monitoring for any adverse effects and adjusting the treatment plan as needed.
Working closely with your healthcare provider is essential when considering ketamine therapy. Your healthcare provider can help ensure your safety, determine the optimal dosage, monitor your progress, identify any drug interactions, and provide follow-up care to monitor the long-term effects of the treatment.
Summary
Ketamine infusion therapy has demonstrated promise as a versatile and effective treatment for various pain conditions and mental health disorders. While not a panacea for all clinical conditions, ketamines unique pharmacological properties and diverse range of applications make it a valuable tool in psychiatry and pain management.
By carefully considering the risks and benefits of ketamine treatment and tailoring the therapy to individual patient needs, it is possible to harness the full potential of this remarkable drug and improve the quality of life for countless individuals struggling with chronic pain, psychiatric illnesses, and substance use disorders.
As research continues to expand our knowledge of ketamine's therapeutic potential, it is crucial for healthcare providers to stay up-to-date on the latest evidence to ensure the safe and effective use of this powerful treatment option. Ongoing efforts to optimize treatment protocols and settings will further enhance the accessibility and efficacy of ketamine infusion therapy for a broader range of patients.
Disclaimer
Anodyne is a multidisciplinary medical centre in Perth Western Australia. With a focus on patient centred and innovative approaches for pain management and mental health recovery.
Any advice posted on our blog, website, or app is of a general nature and for informational purposes only. It is not intended to replace or substitute for any medical or other advice.
Anodyne makes no representations or warranties and expressly disclaim any and all liability concerning any treatment, action by, or effect on any person following the general information offered or provided within or through the blog, website, or app. If you have specific concerns or a situation arises in which you require medical advice, you should consult with an appropriately trained and qualified medical practitioner.
Want to know more?
For more information on ketamine, please go to our comprehensive guide Ketamine Infusion Unveiled: A Comprehensive Guide or visit our Ketamine Resource and Ketamine Therapy pages. If you think ketamine may be a treatment for you, please contact Anodyne to book a consultation with one of our doctors.
See the following articles for some further insights into ketamine infusion therapy:
- https://www.hopkinsmedicine.org/news/newsroom/news-releases/ketamine-isnt-an-opioid-and-treats-depression-in-a-unique-way
- https://www.mayoclinic.org/medical-professionals/psychiatry-psychology/news/ketamine-exploring-continuation-phase-treatment-for-depression/mac-20430307
- https://www.cambridge.org/core/journals/bjpsych-open/article/ketamine-for-the-treatment-of-mental-health-and-substance-use-disorders-comprehensive-systematic-review/36E261BFA62CDA6459B88F7777415FDA